Roughly 2.6 million American adults suffered from an opioid use disorder (OUD) in 2020, according to the National Survey on Drug Use and Health. OUDs can destroy more than just the lives of the people misusing them, and that abuse regularly extends to the workplace. At least 75% of U.S. employers have been directly affected by opioids, which commonly range from prescription medications like OxyContin and Vicodin to “street drugs” like heroin. According to the National Safety Council (NSC), less than 20% of those employers say they feel prepared to deal with the opioid issue, and 55% have no plans to address it. A recovery-supportive workplace can lead to increased productivity, fewer workers compensation filings, fewer injuries, and a drastic decrease in the health care costs associated with employees who misuse opioids.
How can my business develop a recovery-supportive workplace?
One of the most impactful ways a workforce can prevent the potential issues caused by opioid misuse is to try and help prevent instances at work that may perpetuate misuse in the first place. The Centers for Disease Control and Prevention (CDC) recommends some of these preventative measures:
- Decrease difficult working conditions or work demands that might lead to daily or recurrent pain.
- Prevent work-related injuries and illnesses that could lead to the initiation of substance misuse.
- Promote the use of alternatives to opioids for pain management associated with a workplace injury or illness. Opioid pain relievers are among the most prescribed drugs in the country. These drugs have a high potential for misuse, which has led to many overdose deaths and injuries. You may want to consider alternative therapies for pain treatment when designing and reviewing employer-sponsored health care coverage.
- Provide information and access to care for an OUD when it is needed, including access to medication-based or medication-assisted treatment, coupled with individual counseling.
- Provide training to managers and workers to overcome the misunderstanding and bias against individuals with OUD, as well as the words and phrases they should avoid using. This should help reduce the stigma surrounding OUDs and substance use disorders (SUDs) in general.
Additionally, health and wellness topics such as stress management, nutrition and weight management, physical activity and exercise, and pain management are great opportunities to provide educational materials on substance misuse prevention. The training topics can be customized to suit the needs and interests of a specific workplace.
Best practices to instill and maintain a recovery-responsive workplace
The foundation of a recovery-responsive workplace program should be upheld by these pillars, as identified by the Substance Abuse and Mental Health Services Administration (SAMHSA):
- Build a culture of support: If your company employs people who have struggled with substance misuse in the past or who have a family history of substance misuse, try to rally these individuals to create a supportive community within your company. Employees currently struggling with substance use are likely to feel less isolated when there’s a coworker around who can relate to their battle.
- Develop a written policy: Outline a clear, transparent workplace policy regarding substance use that illustrates the reasons for the policy, unacceptable substances and behaviors, the persons covered by the policy, and disciplinary consequences and appeals. Workplace substance use policies should be sensitive to the nature of recovery efforts, according to the CDC, which provides the following example: A recovery-supportive policy will recognize that recovery may involve one or more recurrences and, therefore additional or modified treatment. Since employment increases the likelihood of entering treatment and maintaining recovery efforts, workplace policies should support recovering individuals attempting to maintain employment and gain second-chance employment.
- Educate employees: Recovery-supportive workplaces should provide training to all supervisors and employees. Trainings cover types of drugs, the health impacts of misusing them, how substance use can impact behavior and performance at work, and workplace policies involving substance use. In-person training is recommended as a best practice. Online training should be provided when in-person training is not feasible.
- Utilize employee assistance program (EAPs) and peer support: Instead of focusing mostly on reprimanding employees who are struggling, offer assistance programs. If your company is incapable of offering assistance programs, have resources on hand that can help connect employees with community-based organizations, treatment centers, peer support specialists, helplines, and counselors.
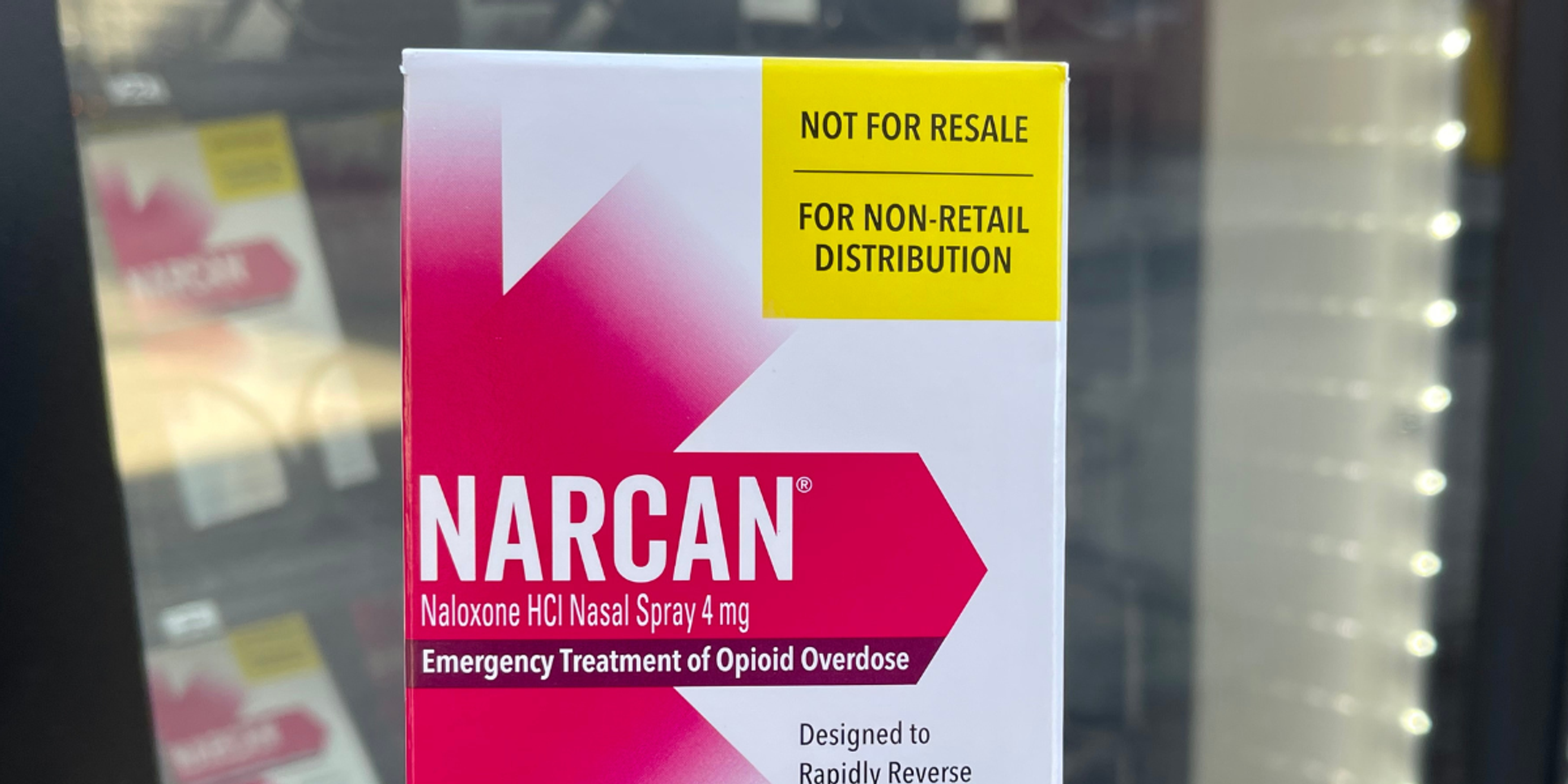
- Place Naloxone in the AED cabinet or even in the restrooms of the building: Even though the focus is on support and recovery this is not always a linear path. Contingency management has its place in preventing adverse outcomes through that journey.
Finding help
The NSC offers employers a free tool kit that includes sample policies, fact sheets, presentations, five-minute safety talks, reports, videos and more to make for a smooth implementation of workplace programs on opioids. Click here to fill out the form needed to receive the tool kit. The CDC also offers numerous workplace resources for companies dealing with OUD in the workplace, including:
- How to use naloxone to reverse opioid overdose
- Infographics and data
- Medication-assisted treatment
- Health hazard evaluation program information
Blue Cross Blue Shield of Michigan and Blue Care Network can help members find an in-network mental health professional by calling behavioral health access lines listed below: PPO: Behavioral Health Access Line | 1-800-762-2382
- A free and confidential resource that’s just a call away when you need immediate support. Behavioral health professionals answer, 24/7.
HMO: Behavioral Health Access Line | 1-800-482-5982
- Connect with a behavioral health clinician if you need help finding a mental health or substance use provider.
- Behavioral health clinicians are available for routine assistance from 8 a.m. to 5 p.m., Monday through Friday. For urgent concerns after hours, clinicians are also available 24 hours a day, seven days a week.
Learn more about mental health and options you have as a member to seek help at bcbsm.com/mentalhealth. More stories for your business:
- Cultivating Relaxation in Daily Life
- Supporting Employees with Autism in the Workplace
- Self-reflection of Your Past 168 Hours
Photo credit: Getty Images