Living with Psoriasis: Effects on Mental Health and Stress
Amy Barczy
| 4 min read
Amy Barczy is a former brand journalist who authored content at Blue Cross Blue Shield of Michigan. Prior to her time at Blue Cross from 2019-2024, she was a statewide news reporter for MLive.com. She has a decade of storytelling experience in local news media markets including Lansing, Grand Rapids, Holland, Ann Arbor and Port Huron.

Grosse Pointe dermatologist Dr. Shauna Ryder Diggs is excited to talk about psoriasis. That’s because the skin condition is so often hidden that some call it an “invisible disease.”
Psoriasis is a lifelong condition, and is often misunderstood by both people who are newly diagnosed with it, and people who don’t have it.
“For people who don’t have it, common misconceptions about psoriasis are thinking it’s an infection or thinking it’s contagious,” said Dr. Diggs, chairwoman of the Board of Directors of the Blue Cross Blue Shield of Michigan Foundation. “Thinking that it’s because someone is dirty or that it is just really bad dandruff and wondering why they aren’t taking care of it.”
While people with psoriasis are at a higher risk for heart disease and type 2 diabetes, they are also at a higher risk for depression and other mental health issues.
What is psoriasis?
Psoriasis is an autoimmune condition that affects 7.5 million people in the U.S. – about 3% of the population. For people with psoriasis, their body’s overactive immune system causes inflammation, which shows outwardly with raised plaques and scales on the skin.
“It’s a condition that you have to control and not cure,” Dr. Diggs said.
The body’s skin cells have a typical life cycle of about a month before they fall off. For people with psoriasis, skin cells have an accelerated life cycle of three to four days; and they pile up on the surface of the skin instead of shedding. For some people with psoriasis, their plaques can sting, burn or itch. This buildup of skin cells is most commonly found on the elbows, knees and scalp. Psoriasis can also cause fatigue; and up to 30% of people with psoriasis also develop psoriatic arthritis.
The causes of psoriasis are not entirely known; it’s believed a combination of genetics and the immune system play a role. There are some common triggers for psoriasis:
- Stress
- Skin injuries, including sunburns, bug bites and scratches
- Illnesses
- Weather
How psoriasis can impact mental health
For those living with psoriasis, the condition can deeply affect their mental health. One study found psoriasis carries the same level of stigma as herpes.
“Because it is a rash that people can see, that alone can have an effect,” Dr. Diggs said. “If you have bad scalp psoriasis, you scratch it all the time, then you get scaling on your clothes. It can cover your nose, face and your eyebrows.”
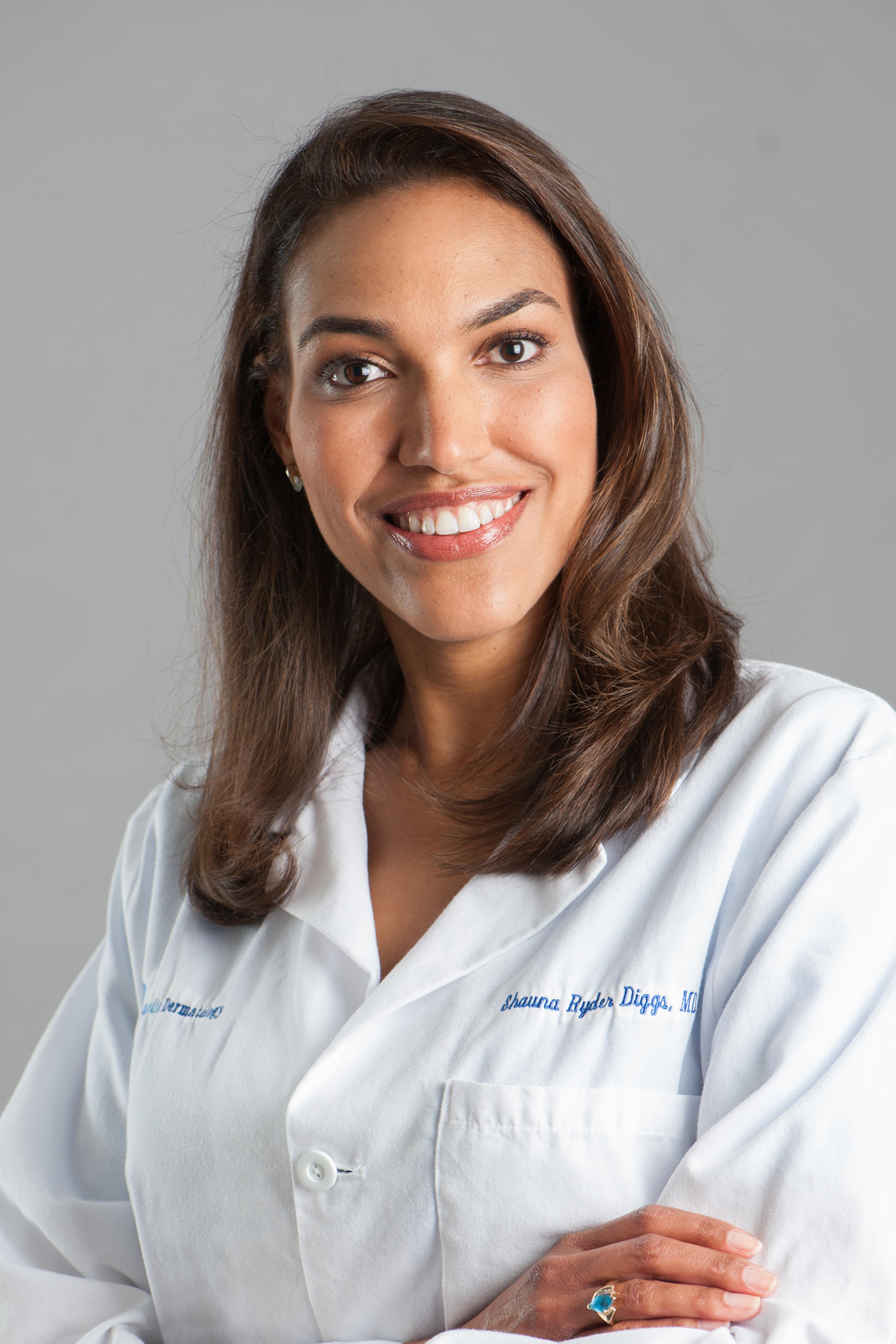
Dr. Diggs said she’s seen how psoriasis affects her patients at her practice, CosmedicDerm in Grosse Pointe.
Often people living with psoriasis try to cover it up; wearing long sleeves in the summertime, for example, or avoiding certain hair styles. It takes time and mental energy to constantly hide.
“It’s a distraction from the other things you want to accomplish in life,” Dr. Diggs said.
At times, people may isolate themselves from others because they are ashamed of their skin. And it can affect personal and sexual relationships.
Often, psoriasis symptoms begin between ages 15 and 25, a time when teens and young adults are particularly vulnerable to body image issues and in a social environment at school where their condition may be misinterpreted and mocked.
However, symptoms can start at any age. Dr. Diggs trained at the University of Michigan, where she said they treated children as young as 6.
Managing stress to manage psoriasis
As an autoimmune condition, psoriasis is something a patient will have to manage and maintain for the rest of their lives. Managing psoriasis takes a combination of a healthy lifestyle and treatment options.
Some treatments like steroid creams are short-term options, while long-term maintenance of psoriasis takes a different treatment approach including topical creams and light therapy.
Lifestyle factors can also help, Dr. Diggs said. Living a balanced, healthy lifestyle with regular movement and a diet that includes omega-3 fatty acids can help. Getting healthy amounts of vitamin D is also good for the skin and can improve psoriasis.
“Sunlight can suppress the immune system,” Dr. Diggs said, noting that 15 to 30 minutes of exposure to sunlight while wearing sunscreen is sufficient for the body’s daily needs to produce vitamin D.
Reducing stress is also a significant factor. That’s because stress is closely related to the body’s inflammatory response – which, when triggered, can cause a flare up of psoriasis; and make itching worse. Finding healthy ways to manage stress is especially important for people with psoriasis.
Some stress management tactics can include:
- Exercise regularly, making sure to consult your doctor before beginning any new exercise regimen
- Practice meditation
- Seek help and counseling
Not only can healthy lifestyle factors help eliminate triggers for psoriasis flare-ups, they can also boost a person’s mental and physical health.





