Knowing the Difference Between Alzheimer's and Frontotemporal Dementia
Jake Newby
| 6 min read
Worldwide, more than 50 million people have dementia. Although there are about 100 types of dementia, most are extremely unusual and rare and unknown to most people. Alzheimer’s disease, the most common type, is responsible for 60-80% of all dementia cases.
Frontotemporal dementia causes about 10 to 20% of the remaining cases and behaves very differently from Alzheimer’s disease. What is the difference between Alzheimer's and dementia?
First, dementia is a general term for a decline in memory, communication, language, and decision-making to the point where it severely affects the ability to function. It is caused by damage to brain cells that affects their ability to communicate, which can in turn affect thinking, feelings, and behavior. It is most common in people over 65 but affects younger people about 5% of the time. It is not a sign of normal aging but a medical disease that can be treated. Making the correct diagnosis is extremely important because many types of dementia are curable or treatable.
Frontotemporal dementia vs. Alzheimer’s disease
Alzheimer’s disease commonly occurs after the age of 70 and affects memory and behavior. The memory loss is unusual though because long term memory is preserved while short term memory is lost. This is confusing for family and friends when the patient can accurately remember what happened 60 years yet cannot remember what happened hours before. It also causes problems with spatial awareness with the patient getting lost in familiar surroundings like the street they live on.
Lastly, as the dementia progresses the patient’s ability to communicate and make good decisions declines until they cannot function. Alzheimer’s disease is incurable but can be treated with medications that can slow down how quickly it progresses.
Frontotemporal dementia (FTD) is caused by progressive nerve cell loss in the brain's frontal lobes (the areas behind your forehead) or its temporal lobes (the regions behind your ears). These are different areas from what occurs in Alzheimer’s disease. It usually occurs earlier than Alzheimer’s disease by about 10- to 20 years and more commonly effects behavior, personality and movement more than memory. FTD can be inherited with about 30% of patients having a strong family history. FTD, which is uncurable but treatable, is broken down into three subtypes:
- Behavioral Variant Frontotemporal Dementia (bvFTD): Characterized by prominent changes in personality and behavior, and judgment.
- Primary Progressive Aphasia: Affects language skills, speaking, writing and comprehension.
- Movement Disorders: Two rare neurological movement disorders associated with FTD are corticobasal syndrome and progressive supranuclear palsy. They occur when the parts of the brain that send messages to the body to perform movement are affected.
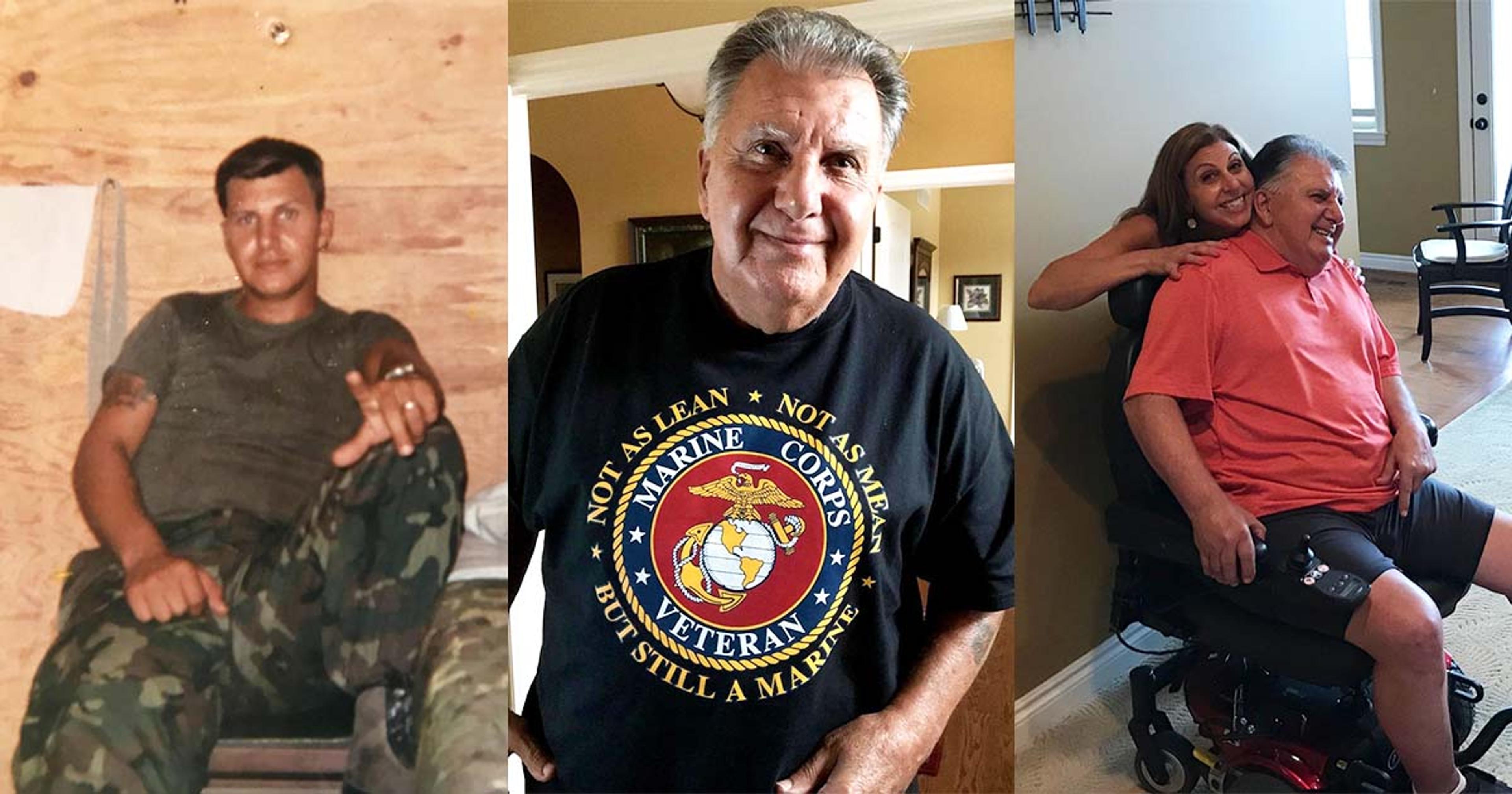
‘A demoralizing and humiliating disease:’ Blue Cross Blue Shield of Michigan (BCBSM) employee shares her family’s fight with FTD
Frank Walkiewicz, the late father of BCBSM Health Care Strategic Communications Manager Shawn Walkiewicz, suffered from corticobasal syndrome, which is caused by corticobasal degeneration. This is a gradual shrinkage and loss of nerve cells in specific parts of the brain that causes progressive loss of the ability to control movement in adults, typically as they reach their 60s.
“He didn’t have memory loss. It was mostly physical,” Walkiewicz said of her father, who succumbed to complications from FTD in 2021. “FTD was not as common years ago as it is now, so he was originally diagnosed with restless leg syndrome. And then it was neuropathy. So, it kind of progressed. At one point in time they said, ‘Maybe it’s Parkinson’s.’”
Walkiewicz said about 10 to 12 years ago, her dad started falling here and there, and each incident would be random. His walking movements also became very stiff and mechanical.
“Our neurologist at the time said part of why my dad didn’t show any symptoms for the longest time is because he was extremely active,” she said. “He was a marine for 27 years, a marine corps drill sergeant. He was a senior Olympian three times. He played racquetball, he played golf and traveled all the time.”
She said when he fell, it took the family a while to put the puzzle pieces together.
“It was almost like he was tripping but it was hard to describe how it happened,” Walkiewicz said. “As the falls were increasing, we were getting more concerned because the injuries weren’t getting worse, but the frequency was increasing.”

Walkiewicz recalls an MRI with a specialist that revealed degeneration to the front part of her father’s brain.
“The way the neurologist described it, which is probably an easy way to explain it, is the brain tells the body what to do, you don’t think about it,” Walkiewicz said. “You never think, ‘I have to blink.’ What’s happening is, the messaging from the brain to the muscle is slowing down or not happening at all and that’s what is causing him to trip. And they told us there would come a time where he wouldn’t blink anymore, because he wouldn’t get the message.”
About a third of all FTD cases are inherited and there are no known risk factors for frontotemporal degeneration apart from family history of a similar disorder. In his final years, Walkiewicz’s dad became immobile and had to be transported throughout his home with the assistance of a Hoyer Lift.
“He could not feed himself, brush his hair, tie his shoes, brush his teeth,” Walkiewicz said. “He couldn’t get out of bed.”
Walkiewicz said she wishes more awareness was brought to FTD. She said members of her family attended a handful of FTD support groups in Troy where other affected families described the personality of their loved one changing because of the disease. Walkiewicz recalled them saying their affected family members got angrier and meaner as they aged. But she had the opposite experience.
“He had a horrible temper when we were younger. He would even say he was mean,” Walkiewicz said. “One of the first signs, but we didn’t see it, was his personality had changed. He was so much fun; he was joking all the time. He never got upset anymore. For us it was like, ‘Finally, he’s relaxed. He’s not so angry anymore.’”
Walkiewicz’s advice for families who begin noticing symptoms like these is to educate themselves; to get online and learn more about FTD, as more information is available than it was 10 to 15 years ago when her father’s signs first sprouted up.
“And also, you have to find yourself a really good neurologist who has experience in all forms of dementia,” she added.
Star actor Bruce Willis was recently diagnosed with FTD at age 67. Walkiewicz said she, like many others, feels awful for Willis and his family. She believes more awareness may be brought to the disease after the high-profile celebrity's diagnosis.
“It is a horrific thing to watch anybody go through it. I’d imagine, even in respect to Bruce Willis, when it’s affecting someone who was so strong and active and physical, to see it get to the point where my dad couldn’t even get to the bathroom – it’s a very demoralizing and humiliating disease,” Walkiewicz said. “Because you’re 100% dependent on others.”
Learn more about frontotemporal dementia from BCBSM Chief Medical Officer Dr. James Grant at this link. You can also find more information on Alzheimer’s disease on MIBluesPerspectives by checking out these articles:
- 5 Myths About Alzheimer's Busted
- What You Need to Know About Alzheimer’s and Other Forms of Dementia
- The Oral Health and Well-Being Connection
Photo credit: Shawn Walkiewicz